Introduction
The private health sector, which includes both for-profit and nonprofit health actors,* is an active and important provider of health information, products, and services.1 More than one-third of modern contraceptive users rely on private sector sources, across 36 low- and middle-income countries. More than 40 percent of caregivers seek care for their sick child in the private sector, across 24 maternal and child survival priority countries identified by the United States Agency for International Development (USAID).2
 Public stewards in many countries are increasingly interested in working with the private sector to achieve health goals, and there is wide recognition that this sector can substantially contribute to increased access to care.3, 4, 5 Inadequate financial and human resources, inefficiencies in the public sector, and increasing uncertainty around future donor commitments have fueled interest in looking beyond the public sector for raising health sector revenue and contributing to public health goals.6, 7 USAID’s further interest in the private sector is marked by its recent private sector engagement policy,8 which recognizes the central role of market-based approaches to achieve sustainable development outcomes. Viewed as an important component of the Journey to Self-Reliance, this policy solidifies the agency’s commitment to encourage public stewards, private enterprise, and donors to co-design solutions to solve development challenges.
Public stewards in many countries are increasingly interested in working with the private sector to achieve health goals, and there is wide recognition that this sector can substantially contribute to increased access to care.3, 4, 5 Inadequate financial and human resources, inefficiencies in the public sector, and increasing uncertainty around future donor commitments have fueled interest in looking beyond the public sector for raising health sector revenue and contributing to public health goals.6, 7 USAID’s further interest in the private sector is marked by its recent private sector engagement policy,8 which recognizes the central role of market-based approaches to achieve sustainable development outcomes. Viewed as an important component of the Journey to Self-Reliance, this policy solidifies the agency’s commitment to encourage public stewards, private enterprise, and donors to co-design solutions to solve development challenges.

Photo: Javier Acebal
While momentum for public-private engagement is building, there is less clarity on how to go about it in an effective way. The USAID-funded Sustaining Health Outcomes through the Private Sector (SHOPS) Plus project seeks to catalyze successful engagement between public and private entities and harness the full potential of the private sector to improve health outcomes. Through its country-based activities, SHOPS Plus found that several factors are essential for effective and sustainable public-private engagement: reliable information about the private health sector, an organized private health sector with a common voice, strong institutional capacity to steward the private sector, and formal agreements between the two sectors with clear roles and responsibilities toward a common objective. Constructive dialogue between the public and private sectors is needed throughout the process.
This brief shares a range of approaches and experiences in public-private engagement from SHOPS Plus’s work with examples from three countries. It provides lessons learned and practical tips for donors who want to support future efforts in public-private engagement in health.
The international community has not yet coalesced around a universal definition of public-private engagement. Three related terms (table) are often used to denote approaches ranging from broad strategies that involve the private sector (private sector engagement) to narrower formal partnerships between public and private entities (public-private partnerships). The ultimate goal of public-private engagement is to contribute to better outcomes by facilitating integration, reducing inefficiencies, and strategically using public and private resources.
| Key terms |
|---|
| Private sector engagement is “a strategic approach to planning and programming through which USAID consults, strategizes, collaborates, and implements with the private sector for greater scale, sustainability, and/or effectiveness of outcomes.”8 |
| A public-private partnership in health is a specific type of public-private engagement that involves “formal collaboration between the public sector at any level and the non-public sector in order to jointly regulate, finance, or implement the delivery of health services, products, equipment, research, communications, or education.”4 |
| Public-private engagement in health is the mutually beneficial collaboration between public and private health sector entities for the purpose of advancing public health goals and achieving sustainable outcomes. |
Public-private engagement on SHOPS Plus takes many shapes and forms depending on country context and local needs. Activities range from supporting NGOs in the Dominican Republic to contract with the national health insurance scheme, to increasing private provider access to government training and family planning commodities in Nigeria, to working with private pharmacies and the Kenyan government to share data through the District Health Information System 2 (DHIS2). This brief discusses four key components of effective public-private engagement (Figure 1) and illustrates lessons using the project’s experience in Senegal, Tanzania, and Nigeria.
A common thread across these components is the presence of frequent and purposeful dialogue between public and private sector actors. Effective dialogue brings stakeholders together to converse, share needs and interests, break down barriers, and resolve bottlenecks.
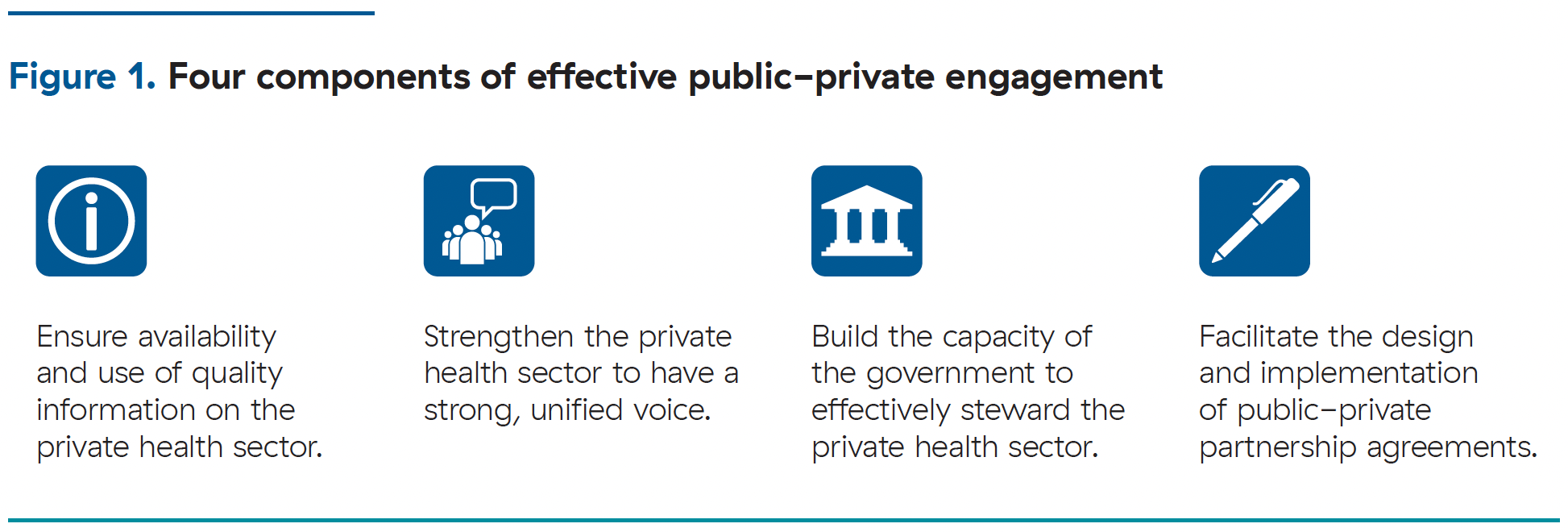 Each case study featured in this brief highlights one of the four components of effective public-private engagement. These components are not mutually exclusive and a country’s public-private engagement approach may focus on one or several of these components, depending on the context and priorities.
Each case study featured in this brief highlights one of the four components of effective public-private engagement. These components are not mutually exclusive and a country’s public-private engagement approach may focus on one or several of these components, depending on the context and priorities.
*The private health sector includes (1) private health providers in for-profit and nonprofit (including faith-based) hospitals, clinics, polyclinics, and doctors’ offices; (2) private pharmacies and drug shops; (3) manufacturers and distributors of health products; and (4) private health insurance schemes.